Reimbursement Systems
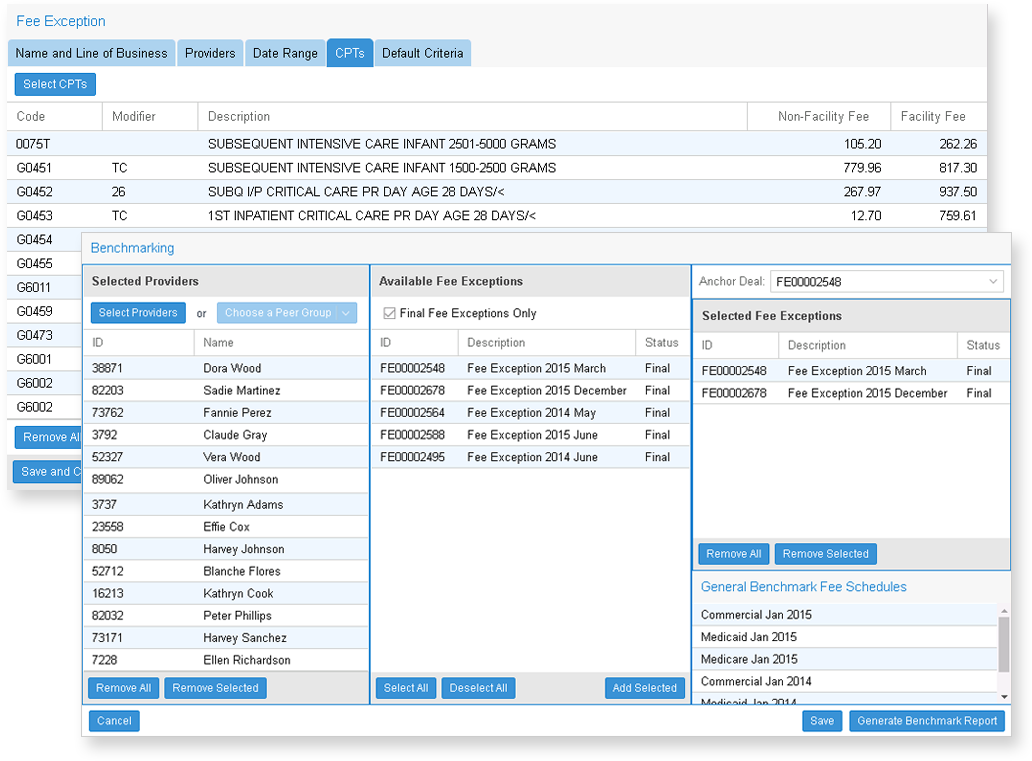
Constant reforms and the myriad of complex payment frameworks make it challenging for payers to stay abreast and current with effective reimbursement systems for providers. Krythium’s Fee Modeler platform is developed based on our extensive experience in designing, developing and implementing successful reimbursement solutions for payers.
Features:
- Cloud-based platform that models reimbursement in real-time using claims data from payers
- End-to-end automation of reimbursement development, modeling, negotiation, implementation, and budgeting process between payers and providers
- Claims experience can be updated frequently providing more reliable models than traditional systems, that often rely on outdated data
- Claims data can be used for modeling as well as for payment validation to ensure that the claims payment system is functioning
- Extensible to value-based reimbursement models using our high-performance HEDIS® and Quality add-on
- Customizable decision dashboards to help monitor and report contracts
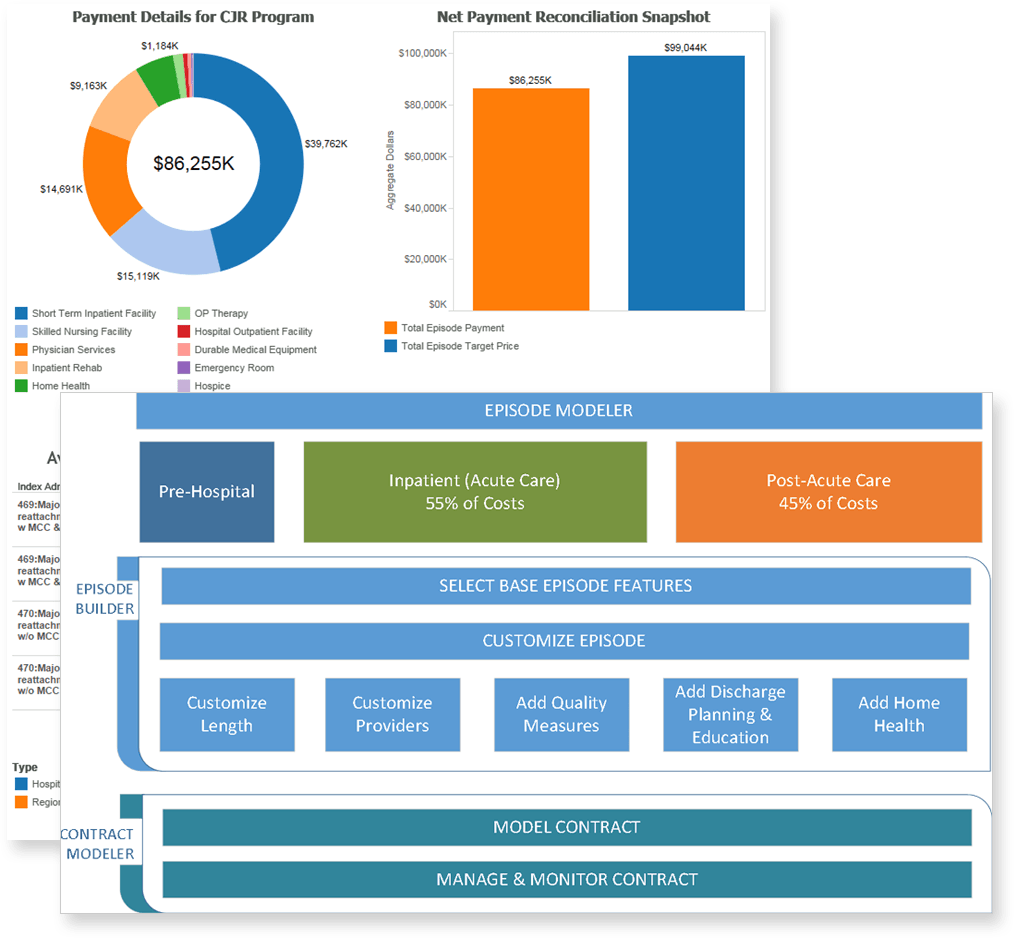
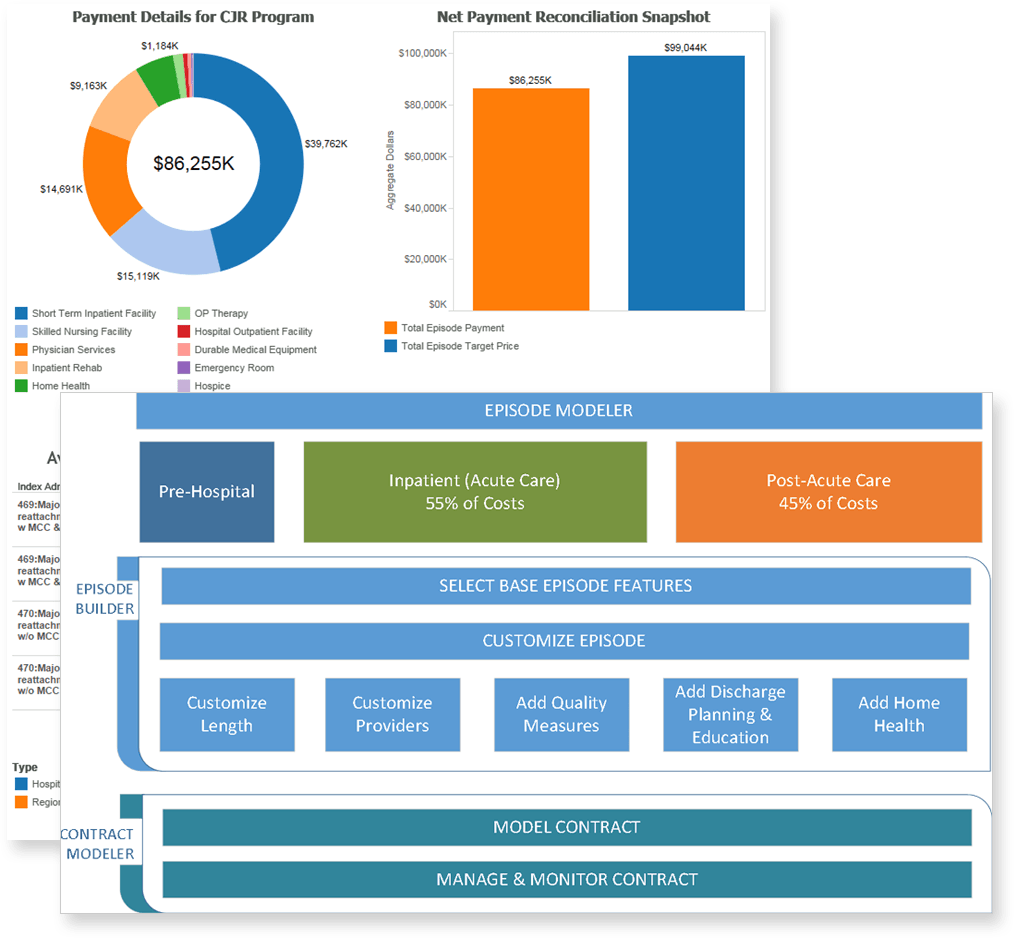
EPISODIC PAYMENT SYSTEMS
Payers can eliminate waste and realign their relationship with providers to realize cost savings and improve quality through our cloud-based Episode Management Platform.
Features:
- Payers can choose pre-configured episode types or build custom episodes that are aligned with objectives
- Costs, Risk and Budget Neutrality can be modeled at real-time using claims data feeds
- Claims data is periodically updated, providing up-to-date models
- Episodes can be monitored using decision dashboards and reporting on episodes
- With the addition of Krythium's quality modules into the contract, the episodes can be monitored for quality parameters resulting in a high quality, value-based payment system
- Through our partnership with Applied Medical Software, a complete end-to-end program for gainsharing can be added, bringing the key aspect of physician alignment to the contract
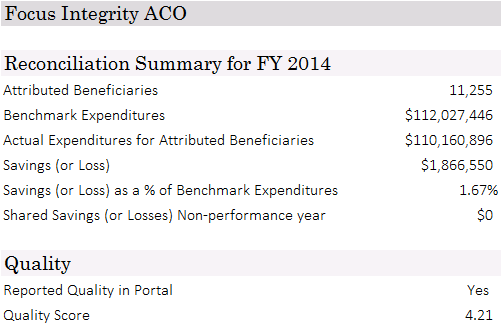
ACCOUNTABLE CARE ARRANGEMENTS (ACAs)
Payers can eliminate waste and realign their relationship with providers to realize cost savings and improve quality through our cloud-based ACA Management Solution.
Features:
- Data is updated frequently providing current information
- The attributed population can be monitored using decision dashboards and reports
- Identification of potential opportunities to reduce costs enables “what-if” modeling to develop a data-driven contract
- Extendable to value-based reimbursement models using our high-performance HEDIS® and Quality add-on module
- Ability to manage quality documentation by obtaining data and charts from providers using our Quality Data Management Solution
- Through our partnership with Applied Medical Software, a complete end-to-end program for gainsharing can be added, bringing the key aspect of physician alignment to the contract
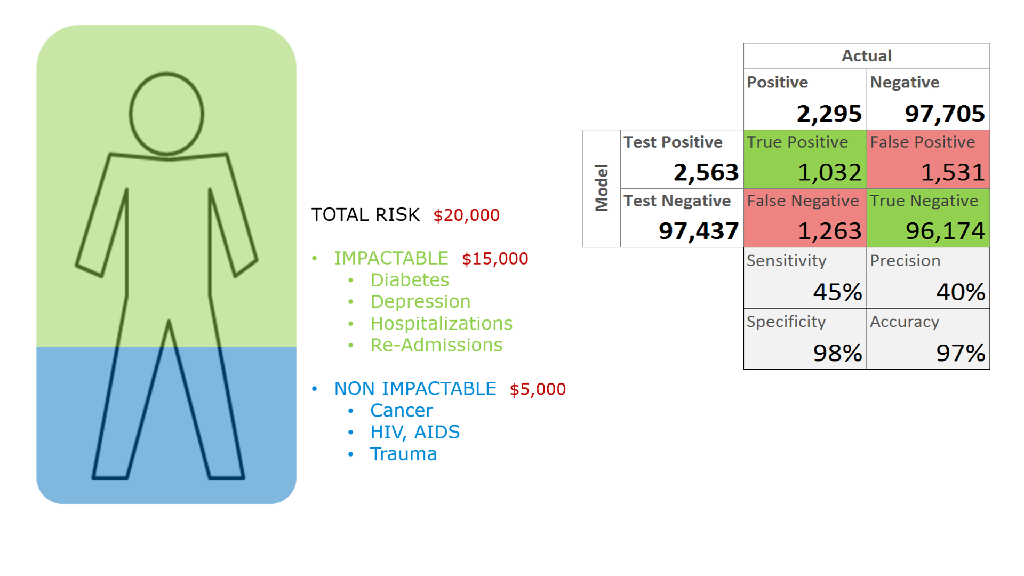
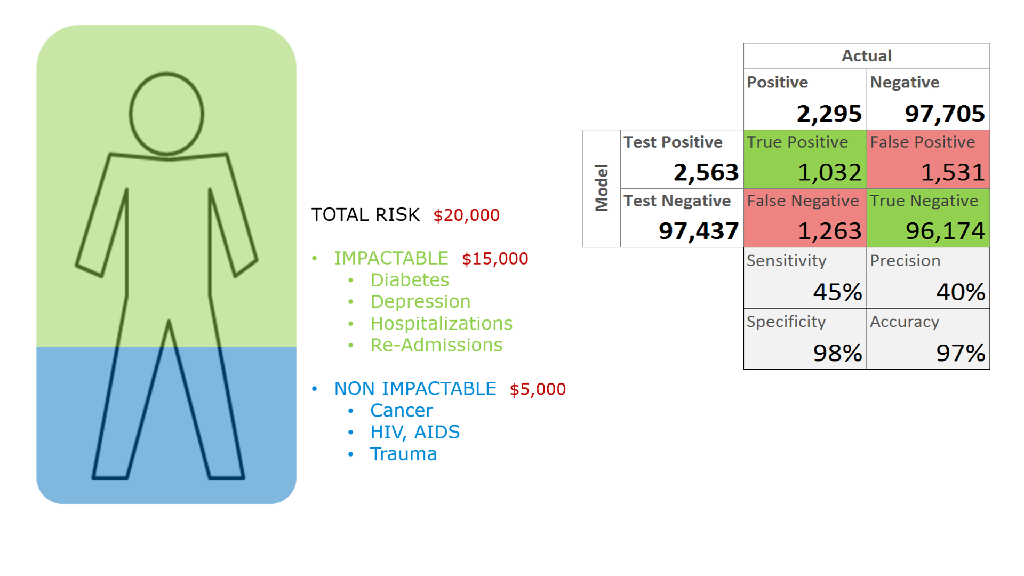
PREDICTIVE RISK MODELING
Payers need more timely, accurate and smarter ways to identify risks associated with their plan and population. This leads to better underwriting and population health management programs. Our predictive analytics platform helps payers identify risks with patient populations quickly and more accurately than available technologies.
Features:
- Predicts risk appropriate for payers program. For example, there is little purpose in using overall cost risk to identify patients who are at risk for readmission
- Predicts actionable and impactable risk when appropriate
- Custom designed algorithms identify risks faster and with higher accuracy
- Uses all available data such as claims, drug, lab and assessment data